A high-level summit regarding superbugs will take place Wednesday at the headquarters of the United Nations (UN) in New York. Scientists have warned for many years that abusing antibiotics create superbugs, which are drug-immune viruses and microbes.
The summit aims to raise awareness of the superbugs’ impact among governments. Bacteria resistance is not simply a medical issue but a threat to national security and a huge economic problem, as suggested by medical experts. The UN has discussed health issues only three times before. The first time was during the HIV crisis of 2011, followed by the summit of chronic illnesses in 2011, where cancer, stroke, diabetes and heart attacks were discussed, and the Ebola summit in 2014.

“There’s a recognition now by different people, different sectors and various organizations that we are, in fact, dealing with an enormous challenge beyond a health issue alone. It doesn’t happen very often for health issues,” said Keiji Fukuda, director of antimicrobial resistance at the World Health Organization.
World efforts
The World Bank believes that under the correct conditions, almost thirty million people from developing countries will enter poverty while low-income countries will lose more than five percent of their GDP by 2050.
Jim O’Neill, a former Goldman Sachs chief economist, chaired an independent British commission that agreed with the World Bank. In this analysis, without taking radical measures to stop superbugs, 100 trillion dollars in economic output will be lost by 2050.
Heads of government and world leaders are supposed to take measures to reduce overuse of antibiotics and other drugs, motivate the development of new medicines, restrict the use of antibiotics in farm animals, and improve access to better diagnostics and treatments.
Thirteen world-leading pharmaceutical companies, including Sanofi, AstraZeneca, and GlaxoSmithKline have presented a “road map” with various objectives they swore to complete in four years to help in the fight against superbugs.
First, they will diminish the environmental footprint generated by antibiotic production, and they will improve access to vulnerable groups to antibiotics, diagnostics, and vaccines.
Pharmaceuticals will also explore new collaborations with the public sphere for research and development, and will share surveillance data on antibiotic’s overuse.
Antimicrobial resistance
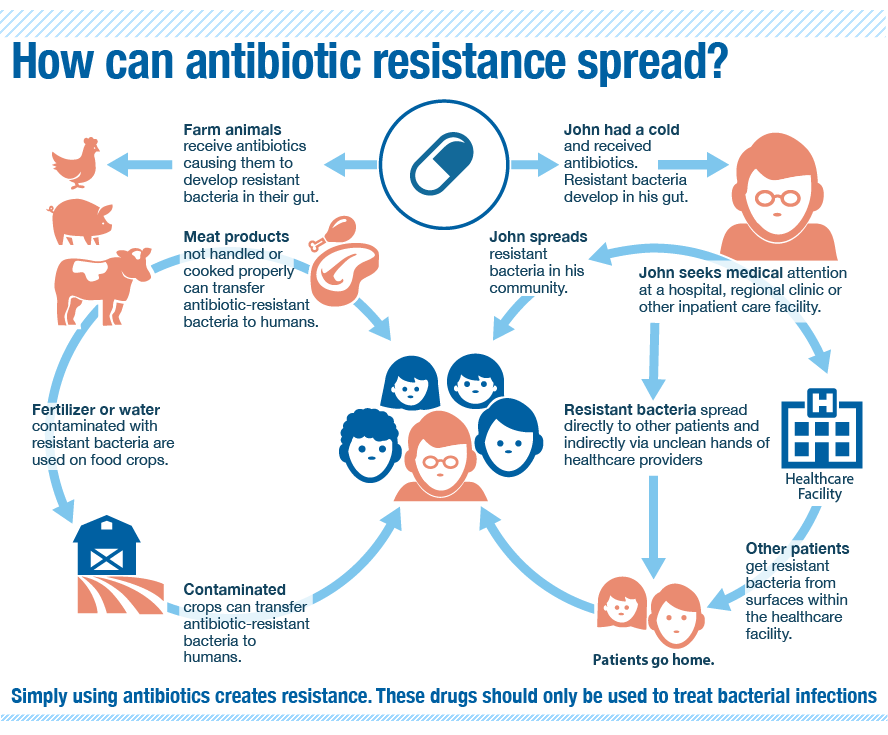
Antimicrobial resistance occurs when a group of viruses and microbes evolves and becomes immune to drugs, including antibiotics. The latter save millions of lives per year.
Antibiotic resistance means that even the simplest infections can be rendered untreatable, shifting medical development back to the 1800s. As stated by the World Health Organization, every year seven hundred thousand people die from antimicrobial resistance.
The Organization believes that if radical measures are not taken, this toll could rise to eleven million deaths per year by 2050, which means one death every three seconds from diseases that used to be treatable.
Only in the United States, it is believed that almost a third of all drugs prescribed by doctors are not needed. Is this abuse of drugs what triggers the evolution of microbes and viruses that become more and more resistant.
The same drugs used in humans are used in farm animals, which later people consume. Specialists expect the United Nations to release a series of standard world objectives to reduce the use of antibiotics to make livestock grow more quickly.
Nonetheless, this will probably make the costs of protein go up since the animals won’t develop fast enough for demand.
“If you want to solve these problems, you need targets and a kind of accountability mechanism to make sure countries do what they say,” said Ramanan Laxminarayan, the director of the Center for Disease Dynamics, Economics & Policy.
Laxminarayan was let down by the UN’s draft resolution that was released this week since it lacks specifications. However, experts praise that the issue is finally being addressed with the seriousness it needs.
High expectations are placed on the summit because world leaders are the only ones with enough power to start mobilizing radical action against superbugs, focusing each on their respective country of origin, according to Allan Coukell, senior director of health programs at the Pew Charitable Trusts.
The “political momentum” for the summit has been simmering for the last couple of years, mostly after various hospitals in Ghana, Africa, were shut down for health risks regarding superbugs. This led the country’s health minister to sponsor a forum on superbugs in 2012.
The United States also announced a plan to combat antimicrobial resistance in 2015, thanks to the Obama administration, which created a presidential council “to combat antibiotic-resistant bacteria.”
Source: The Washington Post
